21 year female with fever
This is an online E logbook to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through a series of inputs from the available global online community of experts intending to solve those patients' clinical problems with collective current best evidence-based inputs.
PRESENTING COMPLAINTS:
A 21 year female presented to the casuality with complaints of :-
1. Fever since 10 AM on 21/07/2022
2. Generalized body pains.
3. Vomiting since evening of 21/07/2022.
HOPI:
A 21 year female presented with complaints of high grade intermittent fever associated with chills and generalized body aches; associated with 6 episodes of vomiting, food as content, non bilious and non projectile associated with abdominal pain. History of frontal headache in a band pattern. History of outside food intake (corn + chicken). No history of bleeding manifestations, tinnitus, cold, cough, chest pain, palpitations, retro orbital pain, SOB, burning micturition, loose stools.
PAST ILLNESS:
Not a k/c/o HTN/ T2DM/ Asthma/ CAD/ CVA/ Epilepsy/ Typhoid/ Thyroid disorders.
PERSONAL HISTORY:
Appetite - Decreased.
Sleep - Adequate.
Allergies:- allergic to Brinjal, Gongura (Roselle leaves) and Potato.
FAMILY HISTORY:
No similar complaints in the family members.
Menstrual History:
Age at Menarche : 12 yrs.
Menstrual cycle : 30/ 3-5 days.
LMP : 22/07/2022.
Associated with Dysmenorrhoea.
IMMUNIZATION STATUS:
Vaccinated as per age.
Vaccinated for Covid 19.
PHYSICAL EXAMINATION:
Ht: 5'2".
Wt: 55kg
No pallor/ cyanosis/ clubbing/ lymphadenopathy/ Icterus/ oedema of feet/ bleeding manifestations.
VITALS:
Patient was conscious and coherent.
Moderately built and nourished.
Temp: 100 F; PR : 88bpm; RR: 19cpm; BP: 110/70 mmHg; SpO2: 98%@ RA; GRBS : 101 mg/dl.
SYSTEMIC EXAMINATION :
CVS: S1, S2 +
R/S : BAE+, Clear
P/A : Soft, Non tender, BS+
CNS :
HMF intact
Power in B/L Upper and Lower limb was 5/5
Reflexes are present with B/L Plantars are flexor.
Fever Chart:-
Investigation chart:-
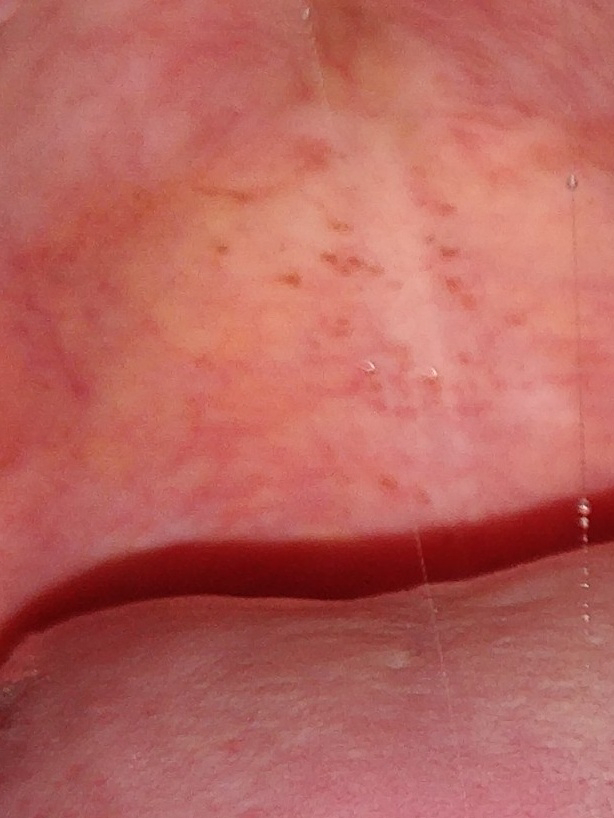
Clinical Images:-
COURSE IN THE HOSPITAL:
A 21 year female presented to the casuality with above mentioned complaints. Upon admission initial examination was done, Hess test was negative; No postural drop; Necessary investigations were done. Patient was shifted to AMC. Dengue for NS1 Ag was positive with negative IgM and IgG; TLC 4800 and Platelets 1.3 L. She was started on IVF and advised to drink plenty of oral fluids. On day 2; she c/o body pains, started having menses associated with Dysmenorrhoea; abdominal pain was decreased; Oral Mefenamic acid was started and IVF and NEOMOL were continued. USG Abdomen was done, which showed no sonological abnormality. On day 3; she had c/o dry cough, headache, Dysmenorrhoea and along with fever spikes. Urine and Blood were sent for Culture and sensitivity. Upon examination postural drop was 18mmHg; PP 34mmHg; on ausculation of lung fields- decreased breath sounds on the Right IAA and ISA when compared to Left lung fields. 1 Unit of SDP transfusion was done on day 4, 1:30 AM i/v/o petechiae and heavy menstrual bleeding. USG Abdomen was done which showed Gall bladder wall edema, Grade I fatty liver, Minimal Ascites at pelvic and perihepatic space. Hess test was negative, No postural drop. She was started on Oral Tranexamic acid + Mefenamic acid. On day 5, as the patient is in Critical defervescence phase of Dengue infection, LFT and RFT were repeated, and the liver enzymes were deranged and Serum Creatinine was 2. Her platelet count was 36,000 and TLC was 4000, upon examination no postural drop, negative Hess test. She was adviced to stop Mefenamic acid and Tranexamic acid. She was tolerating oral feeds. No complaints of bleeding c/m. On day 5, Patient BP was 96/58 mmHg, no postural drop, increase in palatal petechiae, facial puffiness, 2 episodes of stools normal in consistency and colour. On day 6, she was doing good, ambulating, passed stools, no fever spikes/abdominal pain/ nausea and vomiting/ calf pain and headache. She was advised to take plenty of oral fluids. Respiratory examination has decreased breath sounds in Right IAA. Her TLC was 4000, platelets 76000, Sr. Creatinine 0.6. Patient was shifted to Female medical ward. At 5 pm her platelet count was 92000 and TLC 3900, no bleeding manifestations, no postural hypotension and Hess test was negative. On day 7, her menstrual cycle has stopped. Her platelet count 1.5 L and TLC 5100, no fever spikes, appetite improved. She was hemodynamically stable and being discharged in a stable condition.
TREATMENT :
1. PLENTY OF ORAL FLUIDS.
2. IVF NS/RL/ DNS @75ml/hr.
3. INJ. NEOMOL 100ml /IV / SOS.
4. INJ. TRAMADOL 1 AMP IN 100 ML NS / IV / SOS.
5. INJ. PAN 40 MG / IV / OD.
6. TAB. DOXY 100 MG / PO / BD.
7. TAB. PCM 650 MG /PO / TID.
ADVICE AT DISCHARGE :
1. PLENTY OF ORAL FLUIDS
2. HEALTHY DIET INCLUDE GREEN LEAFY VEGETABLES AND FRUITS.
3. TAB. MVT ONCE DAILY AFTER FOOD AT 2 PM.
DIAGNOSIS:
Dengue Hemorrhagic Fever with Thrombocytopenia and Leucopenia.








Comments
Post a Comment