57-year Male with altered sensorium
This is an online Blog book to discuss our patients deidentified health data shared after taking his/ her guardians to sign an informed consent
Here we discuss our patient problems through a series of inputs from the available Global online community of experts with n aim to solve those patient clinical problems with the current best evidence-based input
This Blog also reflects my patient-centred online learning portfolio.
Your valuable input on the comment box is welcome
I have been given this case to solve in an attempt to understand the topic of " Patient clinical data analysis" to develop my competence in reading and comprehending clinical data including history, clinical findings, and investigations and coming up with a diagnosis and treatment plan.
CONSENT AND DEIDENTIFICATION :
The patient and the attendees have been adequately informed about this documentation and the privacy of the patient is being entirely conserved. No identifiers shall be revealed throughout the piece of work whatsoever.
PRESENTING COMPLAINTS:
A 57-year male clinically presented with complaints of:
• Fever for 15 days.
• Pedal oedema and abdominal distinction since 5 days.
• Constipation for 3 days.
• Altered sensorium for a day.
HOPI:
A 57-year male was clinically brought to the casualty with complaints of high-grade intermittent fever associated with chills and rigours for the initial 2 days for which he sought consultation at a local RMP and was treated systematically with oral medications. On day 3 of his illness, he was diagnosed with typhoid and was treated with Intravenous antibiotics for 8 days, he was discharged from the hospital after he got relieved from the symptoms.
History of pedal oedema and abdominal distention since 5 days associated with abdominal pain. History of constipation for 3 days. History of altered sensorium since a day. He was oriented to time, place and person, but has delayed response and is irritable, talking to himself. Now admitted for further management and treatment.
PAST ILLNESS:
Known case of hypertension diagnosed 6 years ago.
Known case of Type 2 Diabetes mellitus diagnosed 6 years ago.
No other comorbidities.
No surgical history.
DRUG HISTORY:
HTN: TAB. LOSAR H 1 tablet once daily after food at 8 AM.
DM: TAB. GLIMI M1 1 tablet once daily after food at 8 AM.
PERSONAL HISTORY:
Moderately built and nourished.
Appetite lost.
Bowels are irregular.
Bladder regular.
No allergies.
Chronic alcoholic (whisky) 180ml once or twice a week.
Chronic smoker stopped 6 years ago after being diagnosed with Hypertension.
GENERAL PHYSICAL EXAMINATION:
The patient was conscious, cooperative and oriented to time, place and person but was an irritable and delayed response to speech.
Pedal oedema of grade II, pitting type.
No pallor, Icterus, cyanosis, clubbing, Lymphadenopathy.
VITALS:
Temp: 99°F; PR: 108bpm; BP: 140/90mmHg; RR: 24cpm; SpO2: %@RA; GRBS: 273mg/dl.
CVS: S1, S2+; R/S: BAE+, fine crept at bilateral IAA; bilateral diffuse rhonchi.
P/A: soft, diffuse tenderness, guarding present.
P/R: No faecal matter noted.
CNS:
GCS: E3V4M6 (13/15)
Moving all limbs.
Reflexes:- Bi. Tri. Su. Knee. Ankle. Plantar
Right:. +2. +2. +1. +3. +1. Flexor.
Left. :. +2. +2. +1. +3. +1. Flexor.
Sensory system : Not elicited.
Cerebellar signs : Not elicited.
No meningiral signs.
Spine examination: Normal.
COURSE IN THE HOSPITAL:
A 57-year male was brought to casualty with the above-mentioned complaints with Foley's catheter in situ. Upon admission, after the initial examination, necessary investigations were sent.
ECG AT PRESENTATION:
CHEST X-RAY AT PRESENTATION:
Viral serology was negative; Hb was 13.8 gm/dl; PCV 39.1%; TLC 24,300 cells/mm³; RBC 4.64 cells/mm³; platelet count 1.01 cells/mm³. ESR 75mmHg in 1st hour; RBS 217 mg/dl; Blood Urea 222mg/dl; Sr. Creatinine 8.0 mg/dl; serum electrolytes were normal; PT 20sec; APTT 39 sec; INR 1.4; CUE showed Albumin of +1; 3-6 pus cells; CRP 2.4 mg/dl (positive); Dengue serology was negative; Sr. LDH 749 IU/L; The patient was started on INJ. MEROPENEM at renal dose modification.
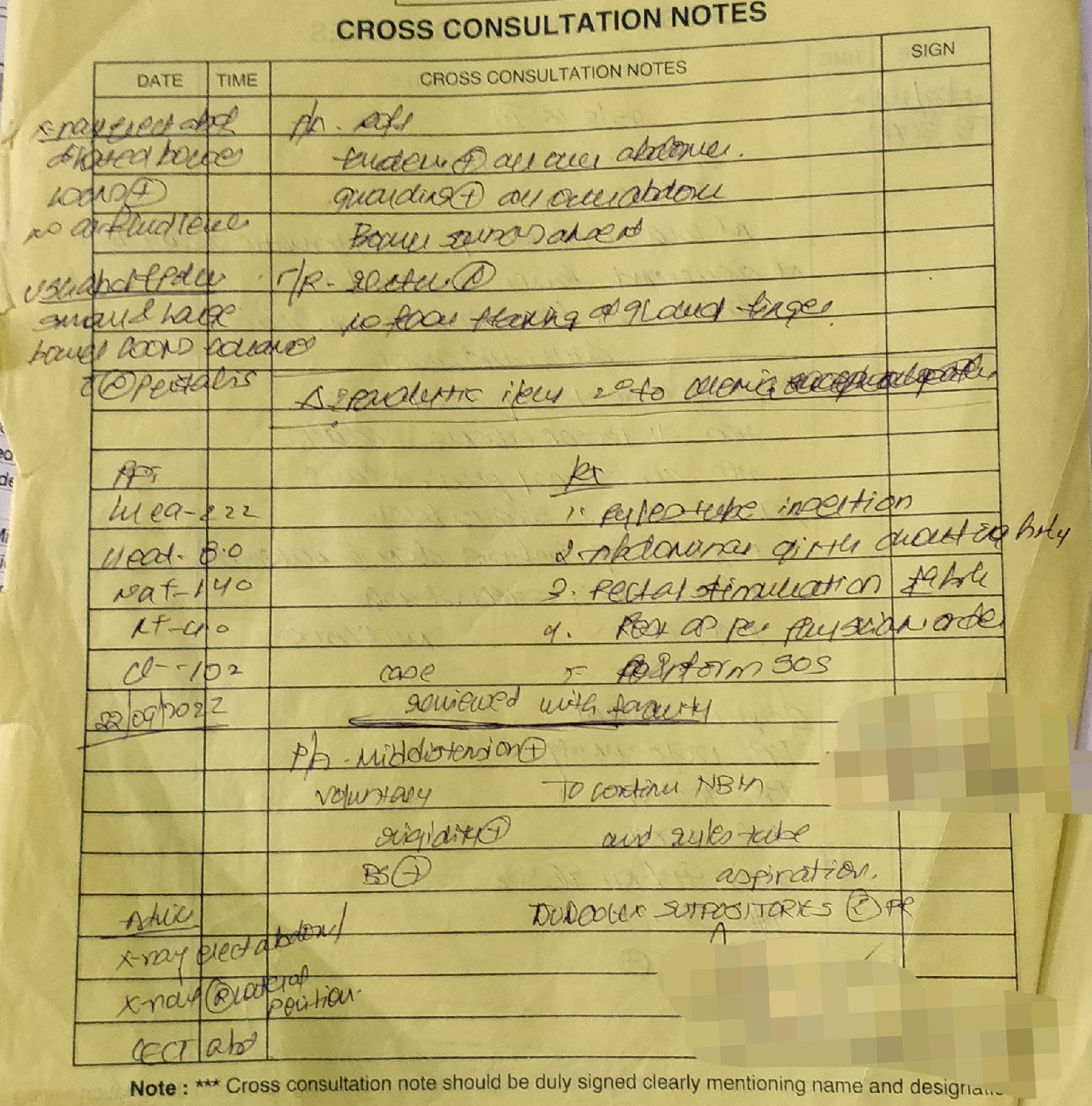
Nephrology cross consultation was taken because of high creatinine levels and orders followed.
General surgery cross consultation was done because of constipation, guarding of the abdomen and absent bowel sounds and orders followed.
USG ABDOMEN was done on 22/09/2022 which showed e/o:
1. Liver of normal size and echotexture with normal CBD and PV. Partially distended gall bladder.
2. Spleen of 13.9 cms with increased size and echotexture.
3. Right kidney 13.2×6.8 cms and left kidney 14.3×6.6 cms with CMD maintained and PCS normal.
4. Prostrate of normal size and echotexture.
With the final impression of:
1. B/L bulky kidneys with altered echotexture and increased AP diameter - s/o AKI.
2. Moderate Ascites.
3. Right mild pleural effusion.
4. Splenomegaly.
On 22/09/22 Left IJV Central line catherization was done under asceptic conditions and the patient was taken up for heparin-free hemodialysis for 4 hours, which was uneventful on 22/09/2022 at 2 AM. Post dialysis his sensorium remains the same. Post dialysis blood urea 137 mg/dl; Sr.Creatinine 4.8 mg/dl; normal serum electrolytes. His abdominal pain and guessing have slightly reduced. Bowel sounds were heard.
RIGHT LATERAL ABDOMINAL X-RAY:
Spot urinary Protein was 34.7 mg/dl and creatinine was 44.1 mg/dl with urinary origin to creatinine was 0.78.
2D ECHO was done on 22/09/2022 which showed evidence of :
Good LV Systolic function; Diastolic dysfunction; No RWMA; No MS/AS; Mild MR; Mild TR and Mild PAH; IVC 1.5 cms dilated and non-collapsing; No PE or LV clots.
2D echo:
The patient was take-up for 2nd session of
hemodialysis which was uneventful on 22/09/2022 at 6 AM. He was started on INJ. N-ACETYLCYSTINE 600mg on 22/09/2022. Post dialysis Blood urea was 58 mg/dl; Sr. Creatinine was 3.3 mg/dl; His sensorium was normal and started on oral feeds. His MODS score was 8.
CECT ABDOMEN was done on 23/09/2022 which showed findings s/o :
1. Mild splenomegaly.
2. Both kidneys are bulky with mild heterogenous enhancement.
3. Mild ascites.
4. Bilateral mild pleural effusions.
http://pacs.kaminenihospitals.com:99/WADO/MetaData?aet=AEKIMS&studyUID=1.2.392.200036.9116.2.6.1.3268.2051739142.1663828405.457566&sessionKey=0003fcd5-9054-48fb-a59b-6697f873d20e&src=Vijaya
Blood and Urine culture and sensitivity showed no growth after 24 hours of incubation.
CNS EXAMINATION:
His blood sugar levels are under control with Inj. Human Actrapid Insulin. 24-hour urinary: volume was 2000ml; Sr. Creatinine was 0.6 g/day; protein was 568 mg/day. Spot urinary: protein was 16 mg/dl; creatinine was 13.2 mg/dl and protein to creatinine ratio of 1.21. During his stay in the hospital, he was treated with Intravenous antibiotics, analgesics and antipyretics and other supportive medications. The patient has been discharged in a hemodynamically stable condition.
CHEST X-RAY ON 24/09/2022
GRBS CHART:
DIAGNOSIS:
SEPSIS WITH MODS ?LEPTOSPIRA (RESOLVED);
RIGHT MINIMAL PLEURAL EFFUSION (RESOLVED);
S/P - 3 HEMODIALYSIS SESSIONS.
1. NORMAL DIABETIC SOFT DIET
2. IVF NS @ 100 ml/ hr
3. INJ. MEROPENEM 500 mg/PO/TID FOR 5 DAYS. ( STOPPED)
4. INJ. DOXY 100 mg/PO/BD FOR 5 DAYS. (STOPPED)
5. INJ. PAN 40 mg/IV/OD
6. INJ. ZOFER 4mg/IV/SOS
7. INJ. THIAMINE 200mg/IV/BD
8. INJ. NEOMOL 1gm/IV/SOS
9. INJ. HUMAN ACTRAPID INSULIN /s/c/TID/acc. to GRBS
10. TAB.CINOD 10 mg/PO/BD.
11. INJ. N.ACETYL CYSTINE 600 mg IN 100 ml NS/IV/TID
12. ZYTEE LOTION FOR @ ORAL CAVITY+TONGUE
13. INPUT AND OUTPUT MONITORING.
14. FEVER AND GRBS CHARTING.
15. VITAL MONITORING.
DISCHARGE MEDICATIONS:
1. STRICT DIABETIC NORMAL DIET.
2. PLENTY OF ORAL FLUIDS.
3. INJ. HUMAN ACTRAPID INSULIN SHOULD BE TAKEN SUBCUTANEOUSLY THREE TIMES DAILY BEFORE FOOD AS 12 UNITS AT 8 AM - 12 UNITS AT 1PM - 10 UNITS AT 8 PM.
4. TAB. CINOD 10 MG 1 TABLET SHOULD BE TAKEN ORALLY TWICE DAILY AFTER FOOD AT 8 AM AND 8 PM.
5. TAB. PAN 40 MG 1 TABLET SHOULD BE TAKEN ORALLY ONCE DAILY 30 MINUTES BEFORE FOOD AT 7:30 AM.
6. TAB. BENFOMET PLUS 1 TABLET SHOULD BE TAKEN ORALLY TWICE DAILY AFTER FOOD AT 8 AM AND 8 PM.
7. HOME MONITORING OF BLOOD SUGAR LEVELS AT 8AM - 1PM - 8 PM.
8. ZYTEE GEL FOR LOCAL APPLICATION OVER THE TONGUE.
Patient was visiting the General Medicine OPD every monthly for follow up and their is no clinical deterioration of his sensorium and renal parameters.
















Comments
Post a Comment